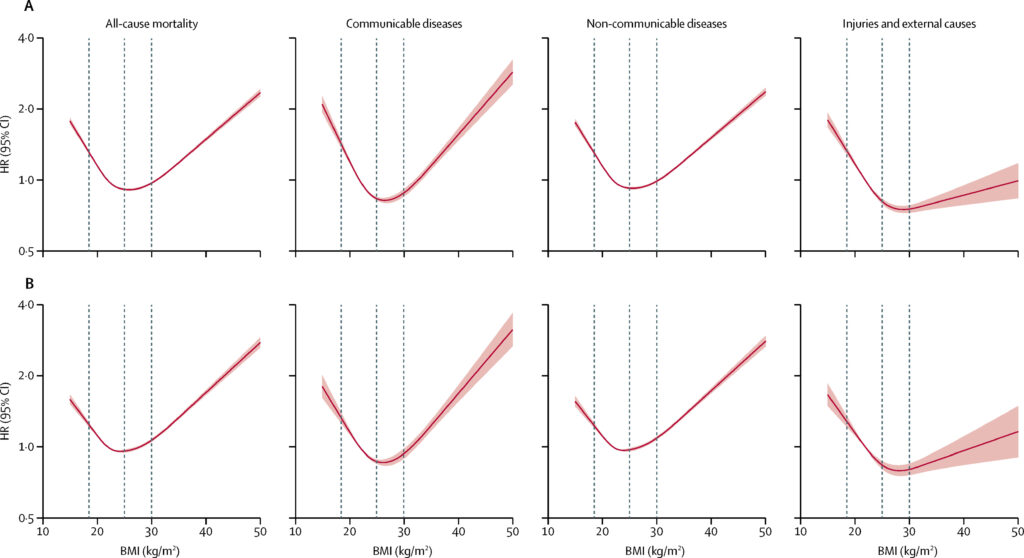
Body Mass Index (BMI) has a significant impact on life expectancy. It affects the way one moves, breathes, thinks. Technically, BMI is a measure of an individual’s body fat and corresponds to weight in kilograms (or pounds) divided by the square of height in meters (or feet). It is often used as an indicator of whether an individual is underweight (<18.5), normal weight (18.5-24.9), overweight (25-29.9), or obese (>30). Ass the figures below illustrate, both low and high BMI values are associated with increased risk of overall and cause-specific mortality1.
Low BMI Affects Life Expectancy
Low BMI is often associated with inadequate nutrition, frailty and underlying health conditions. As such, low BMI is associated with a reduction in life expectancy of about 4.3 years and involves a higher risk of dying from certain causes. Specifically, compared to normal weight individuals, underweight individuals have a higher risk of dying from influenza and pneumonia, suicide2, motor vehicle accident (MVA), fall, septicemia, diabetes, chronic lower respiratory diseases, kidney diseases, cancer (some types) and cardiovascular diseases.
The sections below discuss the underlying mechanisms that make underweight more susceptible to certain causes of death
How Low BMI Affects the Risk of Death from Influenza, Pneumonia and Chronic Lower Respiratory Diseases
- Compromised Immune System: Underweight individuals often have weakened immune systems due to nutritional deficiencies.
- Altered Lung Function: Underweight individuals may have reduced respiratory muscle strength and lung capacity due to insufficient muscle mass. Underweight individuals may also have reduced lung elasticity and lung compliance, making it harder for the lungs to expand and contract properly. Furthermore, these alterations impede the ability of the respiratory system to clear pathogens and increase the risk of respiratory infections.
- Impaired Mucosal Barrier Function: Because of nutritional deficiencies, underweight individuals may experience changes in the integrity and function of the respiratory mucosal barrier which lines the airways and serves as a defense mechanism against pathogens.
- Increased Vulnerability to Stress: Undernutrition is also associated with a diminished metabolic capacity to overcome the amplified physical and psychological demands of illness . Undernutrition is also generally associated with chronic stress which suppresses immune function and increase the risk of respiratory infections.
- Increased Susceptibility to Environmental Factors: Underweight individuals are more vulnerable to environmental factors like pollutants, irritants and allergens that contribute to chronic lower respiratory diseases.
How Low BMI Affects the Risk of Suicide
There is a correlation between low body weight and increased suicide risk but it is important to note that low body weight alone is not a direct cause of suicidal behaviour. Below are some of the reasons why low body mass index is increases the risk of suicide.
- Mental health conditions: Underweight individuals, particularly those with eating disorders such as anorexia nervosa, often experience significant psychological distress. Conditions like depression, anxiety, and body image concerns are commonly associated with eating disorders, and these mental health issues can increase the risk of suicidal ideation and attempts.
- Social and interpersonal factors: Underweight individuals may face social stigma, bullying, or negative comments about their appearance, which can contribute to feelings of low self-worth, social isolation, and an increased risk of suicide. Body image dissatisfaction and societal pressures to conform to certain standards of beauty or thinness can exacerbate these challenges.
- Physical health consequences: Severe malnutrition and physical complications resulting from low body weight can have a detrimental impact on an individual’s overall well-being. The physiological effects of undernourishment can affect brain function and exacerbate mental health conditions, potentially increasing the risk of suicidal thoughts or behaviors.
- Co-occurring factors: Underweight individuals often have co-occurring mental health conditions such as depression or anxiety, which independently contribute to suicide risk. The interplay between these factors can further compound the vulnerability of individuals with low body weight.
How Low BMI Affects the Risk of Death from Motor Vehicle Accidents
- Reduced Body Mass and Protection: Underweight individuals typically have lower body mass and less subcutaneous fat, which provide a certain degree of cushioning and protection during a MVA. The lack of protective layers increases the vulnerability of underweight individuals to injuries.
- Decreased Bone Density: Underweight individuals may have lower bone density and decreased skeletal strength. This makes underweight individuals more susceptible to fractures and severe injuries in the event of a motor vehicle accident, as their bones may be more prone to breaking upon impact.
- Weaker Muscles: Underweight individuals may have reduced muscle mass and overall muscular strength. Strong muscles help stabilize the body and provide some protection during a crash. Weaker muscles may result in reduced ability to withstand forces during an accident, increasing the risk of injury and potential complications.
- Compromised Physiological Reserves: Underweight individuals often have lower reserves of energy and nutrients which compromises their physical resilience and healing abilities. In the aftermath of a motor vehicle accident, underweight individuals may have reduced physiological reserves to cope with the trauma and recover from injuries.
How Low BMI Affects the Risk of Death from Fall
- Reduced Muscle Mass and Strength: Underweight individuals often have lower muscle mass and reduced muscular strength, which affect their balance and stability. Weaker muscles may result in difficulties with coordination and mobility, increasing the risk of falls. In the event of a fall, weaker muscles may not provide adequate support and protection to prevent severe injuries.
- Decreased Bone Density: Underweight individuals often have lower bone density, which is associated with weaker bones. Weakened bones make underweight individuals more susceptible to serious injuries such as fractures. Hip fractures specifically has severe consequences and potentially contribute to mortality.
- Compromised Immune System: as mentioned above, underweight individuals often have weakened immune systems due to nutritional deficiencies. A weakened immune system impairs the body’s ability to recover from injuries sustained in a fall and increase the susceptibility to infections or complications which contribute to mortality.
- Impaired Cognitive Function: Underweight individuals can experience cognitive deficits which affects attention, judgment and decision-making abilities, increasing the risk of falls and severe injuries.
How Low BMI Affects the Risk of Death from Septicemia
- Compromised Immune System: As mentioned above, underweight individuals often have weakened immune systems due to nutritional deficiencies. This make them more susceptible to infections.
- Impaired Wound Healing: Underweight individuals have impaired wound healing due to poor nutrition. Slow or compromised wound healing provides an entry point for bacteria and increase the risk of infections.
- Compromised Physiological Reserves: As mentioned above, underweight individuals often have lower reserves of energy and nutrients which compromises their physical resilience and healing abilities. It is more difficult for and underweight body to mount an effective immune response and handle the systemic effects of an infection.
How Low BMI Affects the Risk of Death from Diabetes
Underweight individuals have a lower risk of developing type 2 diabetes. That is, the majority of individuals with type 2 diabetes are overweight or obese and type 2 diabetes represents more than 90% of people with diabetes. However, an underweight individual with type 1 or 2 diabetes is at an increased risk of complications and mortality from diabetes. The reasons why underweight individuals are more susceptible to death from diabetes than normal weight individuals are the following:
- Glycemic Instability: Underweight individuals with diabetes experience greater glycemic instability, characterized by fluctuating blood sugar levels. Unstable blood sugar levels contributes to complications and increase the risk of mortality.
- Nutritional Deficiencies: As mentioned above, underweight individuals often have nutritional deficiencies. This compromises metabolic control and increases the risk of diabetes-related complications.
- Compromised Immune System: as mentioned above, underweight individuals often have weakened immune systems due to nutritional deficiencies. Infections can be more severe and difficult to treat in individuals with diabetes, leading to an increased risk of complications and mortality.
- Impaired Wound Healing: As mentioned above, underweight individuals have impaired wound healing due to poor nutrition. This reduces their ability to recover from diabetes-related complications such as foot ulcers or infections.
- Weakened Physiological Reserves: Underweight individuals typically have lower physiological reserves, including energy stores and nutrient reserves. Diabetes puts additional stress on the body and underweight individuals may have less capacity to handle the metabolic demands and maintain optimal health. This reduced physiological reserves increases the risk of complications and mortality associated with diabetes.
How Low BMI Affects the Risk of Death from Kidney Diseases
- Nutritional Deficiencies: As mentioned above, underweight individuals often have nutritional deficiencies. Essential nutrients, such as proteins, vitamins and minerals, play a crucial role in maintaining kidney health. Insufficient intake of these nutrients leads to impaired kidney function and structural changes in the kidneys which progresses to chronic kidney disease if left untreated.
- Reduced Renal Reserve: Underweight individuals have reduced renal reserve, which refers to the kidneys’ ability to maintain normal kidney function even under stressful conditions or in the presence of disease. A lower renal reserve makes underweight individuals more susceptible to kidney damage or dysfunction, as the kidneys has less capacity to compensate for stressors or maintain optimal function.
- Compromised Immune System: as mentioned above, underweight individuals often have weakened immune systems due to nutritional deficiencies. This makes them more susceptible to infections that affect the kidneys and contribute to the development of kidney diseases.
- Dehydration: Underweight individuals may have an increased risk of dehydration, which has negative effects on kidney function. Inadequate fluid intake or excessive fluid loss due to factors such as vomiting or diarrhea can lead to dehydration and potentially impair kidney function. Prolonged or recurring episodes of dehydration increases the risk of kidney damage and the development of kidney diseases.
How Low BMI Affects the Risk of Death from Cancer
- Compromised Immune System: As mentioned above, underweight individuals often have weakened immune systems due to nutritional deficiencies. Essential nutrients, such as vitamins, minerals and antioxidants, play important roles in maintaining a healthy immune system and protecting against the development and progression of cancer. The immune system plays a critical role in identifying and eliminating abnormal cells, including cancer cells. When the immune system is weakened, it may be less effective in recognizing and destroying cancerous cells, allowing them to proliferate and develop into tumors.
- Hormonal Imbalances: Underweight individuals may experience hormonal imbalances. Hormones such as estrogen and progesterone influence the development and growth of certain hormone-related cancers, such as breast and ovarian cancers.
- Reduced Body Fat: Underweight individuals typically have low body fat levels, which affects hormone production and regulation. Adipose tissue (fat) is not only an energy storage site but also produces hormones and cytokines that regulate various physiological processes, including inflammation and cell growth. Insufficient body fat levels in underweight individuals disrupts the balance of these hormones and contributes to an increased risk of cancer.
- Impaired DNA Repair Mechanisms: Underweight individuals have impaired DNA repair mechanisms. DNA damage and mutations occur naturally or as a result of environmental factors. Proper DNA repair mechanisms are essential to maintaining genetic stability and preventing the development of cancer.
- Chronic Inflammation: Underweight individuals often experience chronic inflammation, which promotes the development and progression of cancer. Inflammation is a natural response of the immune system to injury or infection, but chronic inflammation has harmful effects on the body. Underweight individuals often have imbalances in pro-inflammatory and anti-inflammatory markers, leading to persistent inflammation that contributes to cancer development.
How Low BMI Affects the Risk of Death from Cardiovascular Diseases
- Compromised Immune System: As mentioned above, underweight individuals often have weakened immune systems due to nutritional deficiencies which contributes to chronic inflammation and the development of cardiovascular diseases.
- Reduced Muscle Mass and Strength: Underweight individuals typically have lower muscle mass and strength. Since the heart is a muscular organ responsible for pumping blood throughout the body, a weaker heart muscle affects its ability to efficiently circulate blood which results in poor cardiovascular function and increase the risk of cardiovascular diseases.
- Hormonal Imbalances: As mentioned above, underweight individuals may experience hormonal imbalances. Hormones play important roles in regulating blood pressure, cholesterol levels and blood vessel health. Hormonal imbalances in underweight individuals affect these regulatory mechanisms and increase the risk of cardiovascular diseases.
- Increased Risk of Arrhythmias: Underweight individuals may be at an increased risk of abnormal heart rhythms due to nutritional deficiencies. Nutritional deficiencies and imbalances in electrolytes, such as potassium and magnesium, affects the electrical signals that regulate the heart’s rhythm. Arrhythmias increase the risk of complications, including blood clots and cardiovascular events.
High BMI Affects Life Expectancy
High BMI is associated with an increased risk of death at an earlier age. Specifically, being overweight (BMI between 25 and 29.9) is associated with an increased risk of death from influenza and pneumonia, drug overdose, kidney diseases, cardiovascular diseases, liver diseases, cancer and fall. Being obese (BMI above 30) further increases the risk of dying from these causes. Specifically, Compared to normal weight individuals, Obese individuals are 100% more likely to dies from influenza and pneumonia, 100% more likely to dies from drug overdose, 94% more likely to dies from kidney diseases, 76% more likely to dies from cardiovascular diseases, 69% more likely to dies from liver diseases, 57% more likely to dies from cancer, 31% more likely to dies from a fall.
The sections below discuss the underlying mechanisms that make overweight individuals more susceptible to certain causes of death
How High BMI Affects the Risk of Death from Influenza and Pneumonia
- Altered Lung Function: Excess body weight affects lung function and respiratory mechanics. Specifically, it leads to reduced lung capacity, decreased chest wall compliance and changes in respiratory muscle strength. These alterations impede the ability of the respiratory system to clear pathogens and increase the risk of respiratory infections.
- Altered Mucus Properties: Excess body weight leads to changes in the composition and properties of respiratory mucus. Mucus in obese individuals tends to be thicker and stickier compared to non-over weight individuals. As such, it is more difficult for overweight individuals to move and clear mucus from their airways.
- Impaired Immune Response: Excess body weight impairs the immune system’s ability to fight off infections. Adipose tissue, commonly known as fat tissues, produces pro-inflammatory molecules that disrupt the normal functioning of immune cells, reducing their effectiveness in combating viruses and bacteria.
- Chronic Inflammation: Excess body weight is associated with a state of chronic low-grade inflammation. This chronic inflammation weakens the immune response and compromise the lung’s ability to clear infections.
- Reduced Vaccine Efficacy: Excess body weight impacts the effectiveness of vaccines. overweight individuals have a reduced response to influenza vaccination and weaker protection against the virus (Sheridan PA, Paich HA, Handy J, Karlsson EA, Hudgens MG, Sammon AB, Holland LA, Weir S, Noah TL, Beck MA. Obesity is associated with impaired immune response to influenza vaccination in humans. Int J Obes (Lond). 2012 Aug;36(8):1072-7. doi: 10.1038/ijo.2011.208. Epub 2011 Oct 25. PMID: 22024641; PMCID: PMC3270113.).
How High BMI Affects the Risk of Death from Drug Overdose
- Higher Medication Dosing: In some cases, medications are prescribed based on a person’s body weight. Overweight individuals may require higher doses of certain medications to achieve the desired therapeutic effect. As the dose makes the poison, overweight individual have a higher risk of accidental overdose.
- Metabolic Changes: Excess body weight leads to changes in adipose tissue distribution, liver function and renal clearance which affects the absorption, distribution, metabolism and excretion of medications. These changes can impact drug levels in the body, potentially increasing the risk of overdose.
- Polypharmacy: Polypharmacy refers to the use of multiple medications. Excess body weight is associated with comorbidities that are often treated with sedative medications such as opioids or benzodiazepines. For example obesity is a significant risk factor for obstructive sleep apnea (OSA) and OSA is often treated with sedative medications. Excess body weight is also associated with an increased risk of mental health conditions, such as depression and anxiety which are often treated with benzodiazepines that are associated with an increased risk of overdose, particularly when taken in excessive amounts or combined with other substances, such as alcohol or opioids. As such, overweight individuals may be prescribed multiple medications to manage their health and the use of multiple medications increases their risk of overdose because of drug interactions or the combined effect of different drugs.
How High BMI Affects the Risk of Death from Kidney Diseases
- Diabetes and Insulin Resistance: Excess body weight is closely linked to insulin resistance and the development of type 2 diabetes. Diabetes is a leading cause of kidney disease, known as diabetic nephropathy. Excess body weight and insulin resistance lead to high blood sugar levels, causing damage to the small blood vessels in the kidneys over time.
- Hypertension: Excess body weight is a significant risk factor for hypertension (high blood pressure). The excess weight puts additional strain on the cardiovascular system, leading to increased blood pressure. Chronic hypertension damages the blood vessels in the kidneys and impair their function, eventually leading to kidney disease.
- Chronic Inflammation: Excess body weight is associated with a state of chronic low-grade inflammation as adipose tissue produces inflammatory molecules. This chronic inflammation contributes to kidney damage and the development of kidney diseases.
- Adipokine Dysregulation: Adipose tissue produces various hormones and signaling molecules, known as adipokines. Excess weight leads to a dysregulation of adipokines, such as leptin and adiponectin, which affects kidney function. Dysregulated adipokine levels contribute to inflammation, oxidative stress and fibrosis in the kidneys, increasing the risk of kidney diseases.
- Dyslipidemia: Excess body weight is often associated with dyslipidemia, characterized by abnormal levels of cholesterol and triglycerides in the blood. Dyslipidemia contributes to the development of atherosclerosis and vascular damage in the kidneys, leading to impaired kidney function and an increased risk of kidney diseases.
- Obstructive Sleep Apnea (OSA): Excess body weight is a significant risk factor for OSA, a condition characterized by interrupted breathing during sleep. OSA is associated with an increased risk of kidney damage because of the repeated episodes of oxygen deprivation and the resulting stress on the kidneys.
How High BMI Affects the Risk of Death from Cardiovascular Diseases
- Elevated Blood Pressure: Excess weight and adipose tissue leads to hypertension (high blood pressure). The heart has to work harder to pump blood through the body, which strains the cardiovascular system and increases the risk of CVDs like heart attacks and strokes.
- Dyslipidemia: As mentioned above, excess body weight is often associated with dyslipidemia, characterized by abnormal levels of cholesterol and triglycerides in the blood. Overweight individuals may have higher levels of LDL cholesterol (often referred to as “bad” cholesterol) and lower levels of HDL cholesterol (often referred to as “good” cholesterol). This lipid profile is associated with an increased risk of atherosclerosis (the buildup of plaque in the arteries), which leads to heart disease and strokes.
- Insulin Resistance: excess body weight is closely linked to insulin resistance, a condition in which the body’s cells become less responsive to the effects of insulin. Insulin resistance is associated with an increased risk of CVDs, as high blood sugar levels damage blood vessels and contribute to atherosclerosis.
- Chronic Inflammation: As mentioned above, Excess body weight is associated with a state of chronic low-grade inflammation as adipose tissue produces inflammatory molecules. Chronic low-grade inflammation is associated with atherosclerosis, endothelial dysfunction and plaque formation in the arteries, increasing the risk of CVDs.
- Vascular Dysfunction: Excess body weight impairs the function of blood vessels, leading to endothelial dysfunction. The endothelium is the inner lining of blood vessels and when it becomes dysfunctional, it contributes to the development of atherosclerosis and the formation of blood clots.
- Sleep Apnea: As mentioned above, excess body weight is a significant risk factor for OSA, a condition characterized by interrupted breathing during sleep.. Sleep apnea is associated with an increased risk of hypertension, heart failure and other CVDs.
- Adipokine Dysregulation: As mentioned above, adipose tissue produces various hormones and signaling molecules, known as adipokines. Excess weight leads to a dysregulation of adipokines which contribute to chronic inflammation, insulin resistance and endothelial dysfunction, all of which are associated with an increased risk of CVDs.
- Hypertension: Excess weight is a significant risk factor for hypertension (high blood pressure) which increases the workload on the heart and strains the cardiovascular system which increases the risk of heart disease.
How High BMI Affects the Risk of Death from Liver Diseases
Obesity is a significant risk factor for the development of liver diseases, including non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH). Several underlying mechanisms contribute to the increased susceptibility of overweight individuals to liver diseases:
- Insulin Resistance: As mentioned above, excess body weight is closely linked to insulin resistance, a condition in which the body’s cells become less responsive to the effects of insulin. Insulin resistance promotes the accumulation of fatty acids in the liver, leading to the development of NAFLD. Elevated insulin levels also stimulate the production of liver fat and promote inflammation, which can progress to NASH.
- Lipid Accumulation: Excess body weight and abdominal obesity contribute to increased levels of circulating free fatty acids and triglycerides. These lipids are taken up by the liver, leading to the accumulation of fat within liver cells. Over time, excessive lipid accumulation causes inflammation and liver cell damage.
- Chronic Inflammation: As mentioned above, Excess body weight is associated with a state of chronic low-grade inflammation as adipose tissue produces pro-inflammatory molecules. This chronic state of inflammation contributes to liver inflammation and injury.
- Oxidative Stress: Excess weight is associated with increased oxidative stress, which occurs when there is an imbalance between the production of reactive oxygen species (ROS) and the body’s ability to neutralize them with antioxidants. Oxidative stress damages liver cells and promote inflammation and fibrosis, leading to liver disease progression.
How High BMI Affects the Risk of Death from Cancer
- Chronic Inflammation: As mentioned above, excess body weight is associated with a state of chronic low-grade inflammation as adipose tissue produces pro-inflammatory molecules. Prolonged inflammation contributes to the development and progression of cancer.
- Hormonal Imbalances: Adipose tissue produce hormones such as estrogen, insulin and insulin-like growth factors (IGFs). In overweight individuals, these hormones may be present in higher levels, which promotes cell growth and division, potentially increasing the risk of certain hormone-related cancers, such as breast and endometrial cancer.
- Insulin Resistance: As mentioned above, excess body weight is closely linked to insulin resistance, a condition in which the body’s cells become less responsive to the effects of insulin. Insulin resistance leads to increased insulin levels in the blood, which promotes cell growth and potentially contribute to the development of certain cancers.
- Altered Adipokine Levels: Adipose tissue produces adipokines, which are involved in regulating various physiological processes, including inflammation, cell proliferation and angiogenesis (the formation of new blood vessels). In obesity, the levels of adipokines, such as leptin and adiponectin, may be dysregulated, potentially promoting cancer development.
- Changes in Immune Function: Excess body weight affects the immune system and its ability to respond to cancer cells. Adipose tissue release certain immune-modulating substances, altering the immune response and potentially impairing the body’s ability to detect and eliminate cancer cells.
- Oxidative Stress: As mentioned above, excess weight is associated with increased oxidative stress, which occurs when there is an imbalance between the production of reactive oxygen species (ROS) and the body’s ability to neutralize them with antioxidants. Prolonged oxidative stress causes DNA damage and genetic mutations, which are associated with an increased risk of cancer.
How High BMI Affects the Risk of Death from Fall
- Impaired Balance and Coordination: Excess body weight affects an individual’s balance and coordination. The extra weight puts additional stress on the musculoskeletal system, making movements more challenging and potentially impairing balance. This increases the likelihood of falls, particularly in situations requiring quick adjustments or changes in body position.
- Decreased Muscle Strength: Excess body weight is associated with reduced muscle strength, particularly in the lower extremities. Weakened muscles may lead to difficulties with activities such as walking, climbing stairs, or maintaining stability. Inadequate muscle strength compromises balance and increase the risk of falls.
- Joint Problems and Pain: Excess body weight is often associated with joint problems, such as osteoarthritis. Joint pain and stiffness limits mobility and increase the risk of falls, especially if they affect weight-bearing joints like the knees or hips. Chronic pain also lead to alterations in gait patterns and stability.
- Impaired Proprioception: Proprioception refers to the body’s ability to sense its position and movements in space. Excess body weight impairs proprioceptive feedback, making it more challenging for individuals to maintain balance and react appropriately to changes in posture or surface conditions.
- Reduced Flexibility: Excess body weight is associated with reduced flexibility and range of motion in joints, limiting an individual’s ability to adjust their body position and maintain stability. Decreased flexibility may make it more difficult to recover from a trip or stumble, increasing the risk of falling.
- Cardiovascular Issues: Excess body weight is often linked to cardiovascular conditions such as hypertension and reduced cardiovascular fitness. Cardiovascular problems result in dizziness, lightheadedness, or reduced oxygen supply to the brain, potentially leading to falls.
Closing Remarks
As presented above, BMI is a cornerstone of health. Managing and controlling weight is instrumental to preserving life expectancy and can be achieved with lifestyle modifications like adopting a healthy diet, engaging in regular physical activity and managing stress.
Predicting life expectancy is complex and needs to take many factors into consideration. Youlldie allows to visualize how body mass index interacts with other factors like gender, race, world region, income, education, alcohol, tobacco, physical activity, sleep, blood pressure and family history to statistically predict life expectancy.
References
- Bhaskaran K et al. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. The Lancet. Diabetes and Endocrinology. 30-Oct-2018. https://doi.org/10.1016/S2213-8587(18)30288-2
- Kim H, Jeon HJ, Bae JN, Cho MJ, Cho SJ, Lee H, Hong JP. Association of Body Mass Index with Suicide Behaviors, Perceived Stress, and Life Dissatisfaction in the Korean General Population. Psychiatry Investig. 2018 Mar;15(3):272-278. doi: 10.30773/pi.2017.06.28. Epub 2018 Feb 28. PMID: 29486542; PMCID: PMC5900366. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5900366/